Article reposted from Gwinnett Prep Sports
Author: Christine Troyke
Eddie Knox, who grew up in Augusta, is the athletic trainer at Mountain View and in his second year as a teacher at Grayson. He got his degree at Valdosta State, during which time he worked for the Tampa Bay Buccaneers during consecutive summers. As a senior, Knox accepted an intership at Sports Medicine South in Gwinnett and was later hired full-time.
In this installment of “Getting to Know …,” Knox talks with staff writer Christine Troyke about a variety of topics, including growing up in a military family, bringing pro-level care to high school athletes and the one TV show he DVRs.
CT: Where did you grow up?
EK: Kind of everywhere. I’m a military child. I was born in Virginia, but if I was to say I grew up anywhere, it would probably be Augusta. My dad was stationed at Fort Gordon. But right here in Georgia is where I’ve spent most of my life.
CT: How long were you in Augusta?
EK: Close to 14 years. We traveled around in Germany, but I was really young at that point. My dad was in the Army for about 23 years. We were stationed at Fort Lee in Virginia for three years and after that is when we went to Germany. He did a tour there for two years. Shortly after that is when we officially moved to Fort Gordon. Luckily enough, we were able to stay in Augusta. I was there from elementary school through high school.
CT: What sports did you play?
EK: Football, track and field, and basketball.
CT: What was your best sport?
EK: The sport I was getting recruited in was football and then also track and field.
CT: Looking back, how would you scout yourself?
EK: I was a do-it-all football player. I definitely wasn’t a three- or four-star like some of these guys in Gwinnett County, but I was a do-it-all hard worker. I was easy to get along with — Yes, sir. No, sir — and coaches liked that.
CT: What was your college decision-making process like?
EK: Ultimately I knew I wanted to do something in medicine. I didn’t know exactly what I wanted to do in the field, but selecting colleges, No. 1, I wanted to move as far away from home as I could. (laughing) So that was Valdosta. But also, at that point, I was still interested in the military and they had a good ROTC program there. For that reason and also because they had a strong athletic training/sports medicine program, I decided to go down there.
CT: When did you figure out athletic training was really the direction you wanted to go?
EK: Probably my sophomore year. I started out as premed and then after more research and talking to people, you understand medical school is like 16 years. I didn’t know if I was quite ready for that, at that age.
CT: And a truckload of debt.
EK: I definitely took that into consideration. I love sports and I love medicine. Athletic training is born out of that.
CT: What was your first job ever?
EK: (laughing) I was an apprentice with an electrician. Way back then, I thought that’s what I wanted to do. I came from a blue-collar family. My best friend’s dad was an electrician. He owned his own business. So I would ride around Augusta with him in a 1976 Chevy van and I would do simple stuff. It was a really cool thing. I actually loved it.
CT: What was your first job out of college?
EK: I came up here to Atlanta and started working in an orthopedic office with Dr. (Gary) Levengood. I was an athletic trainer doing clinical outreach. I started there first and branched out into the community from there.
CT: How long ago was that?
EK: Close to nine years. I was there from 2009 until just this past year.
CT: What precipitated the move to Mountain View?
EK: I’ve always done clinical outreach and Mountain View has been my school as far as sports medicine care for about eight years. But what I would do is work in the morning in the clinic and then come here to take care of the sports medicine program.
CT: Now you’re just here?
EK: No, I teach now. That’s something new. I actually teach sports medicine at Grayson High School.
CT: I didn’t know sports medicine was an option. How long have they offered that?
EK: For a while. There are two type of sports medicine classes, but to make it easy, I’d say close to 15 to 20 years. Sports medicine has really changed over the years so they continue to add in curriculum.
CT: What appeals to you about working with high school athletes? You’ve worked at all levels, college and also with the Tampa Bay Bucs.
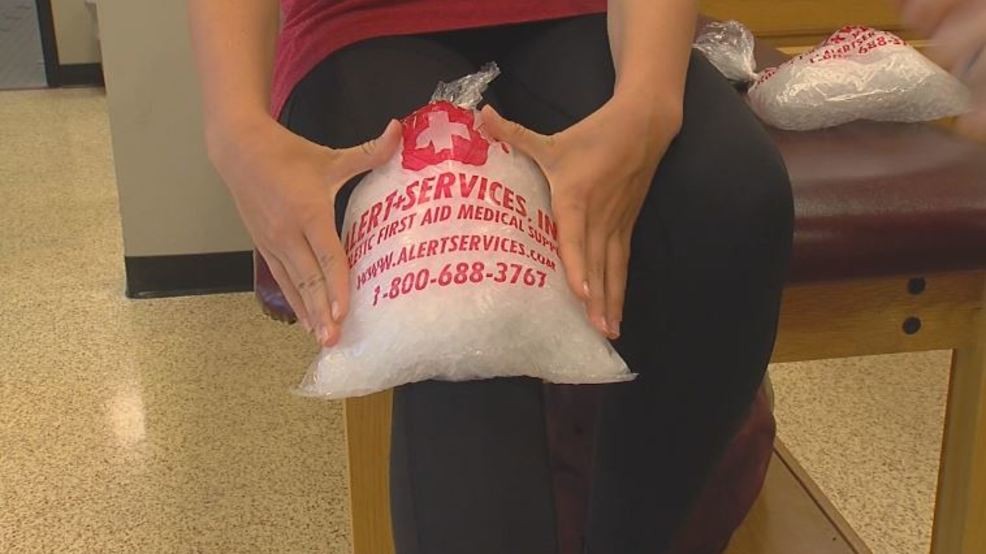
EK: There’s so much opportunity for better care at the high school level. That’s really what motivates me. When you look at other (levels), they really have everything they need. The major Division I and II colleges, they’ve got everything. So how can we assimilate what they have at the NFL and college level and help bring that to high school athletes? They’re the most vulnerable to injuries.
CT: Is the hardest part of the job getting an athlete to admit they’re hurt?
EK: (chuckling) If they’re an athlete, yeah, it’s hard to get them to admit if they’re hurt. But every athlete has a different personality and it’s trying to match their personality with your skill of care. It’s important. You may have an athlete that’s really aggressive that wants to get back on the field where we have to meet our skill of care to that.
CT: It’s interesting how coaching and athletic training run parallel in ways, especially when it comes to sports psychology and understanding how athletes are motivated.
EK: No doubt about it. Actually, the history of athletic training, 50 years ago, before we really saw official certification, a lot of coaches were athletic trainers. It’s natural. Everybody here calls me Coach Knox.
CT: Is this your first year teaching?
EK: Second.
CT: How’s it going?
EK: I love it. I love mentoring kids and to me, it’s not just about teaching, it’s about connecting kids and helping them toward their future. I really love it.
CT: What was it like working for the Bucs?
EK: That was actually done, they had a program with the Bucs, and I really credit our program director at Valdosta State, Russ Hoff. He really was the one that directed me and gave me the opportunity to work down at Tampa Bay. It really gives you an idea of what it’s like to work in the NFL. One thing I got out of it is it’s a lot of work. You’re trying to add small systems to large systems.
It was definitely an experience I will always remember. I gained a lot of experience on how to conduct myself professionally and what hard work means. Then how is information communicated throughout the team. But working there was awesome.
I’ll never forget the first hit that I heard. It sounded like a trainwreck. It was amazing. You appreciate the game and sport at that level. It’s different than watching it on TV.
CT: And like you said, the level of care is unparallelled.
EK: They have everything. They had just renovated the whole facility. They have everything you can thing of to make sure the athletes stay safe and healthy.
CT: Were you a senior when you interned with Sports Medicine South?
EK: It was an externship. So for a whole year, I was still in school, but I was off campus in Atlanta. It was their way of getting on-the-field experience and 12 credits at the same time.
CT: Can you detail all of your responsibilities when it comes to this job?
EK: (laughing) Oh, man. I can give you the five domains: prevention, treatment, recognition of injuries, administration and management. Whatever you can think of that falls under that is what we do. We do everything on behalf of the athlete.
Athletic training has really evolved, I think for the better. It’s a lot of responsibility, but it’s a lot of things we do for the kids to make sure they have a safe environment to play and practice in.
CT: What kind of music do you listen to most often?
EK: I love 2000s hip-hop. That’s my era. Kendrick Lamar is really big on my list right now. We actually just recently saw him in concert. I love country, too. Now, I couldn’t tell you a country artist’s name, but I turn on the station and jam out. I listen to everything honestly.
CT: Who would you like to see in concert if money were no object?
EK: If I could bring them back, I would probably say Tupac. He was talking about real stuff that was happening in society.
CT: Are there TV shows you DVR?
EK: I don’t really have time to watch TV, but the one show I do DVR is “ABC World News.” That’s the one show I watch when I get home because I have to figure out what’s going on.
CT: Are there movies you will always watch?
EK: “Rush Hour.” It’s one of my favorites of all time.
CT: How many U.S. states have you been to?
EK: Really, not that many. Maybe about seven. All along the eastern seaboard.
CT: Is there a part of the country you haven’t seen that you would like to?
EK: I would love to go up to Maine and that area. The scenery up there has to be awesome — and I love seafood. That’s the main thing (laughing).